Absence doesn’t make the heart grow fonder: an interesting case of partial pericardium.
Dr Tom Chance1, Dr Laura Duerden1, Dr Jonathan Rodrigues2, Dr Stephen Lyen1, Dr M Hamilton1, Dr N Manghat1.
Affiliations:
1 Department of Radiology, Bristol Royal Infirmary, United Kingdom
2 Department of Cardiothoracic Imaging, Toronto General Hospital, Toronto
Image focus:
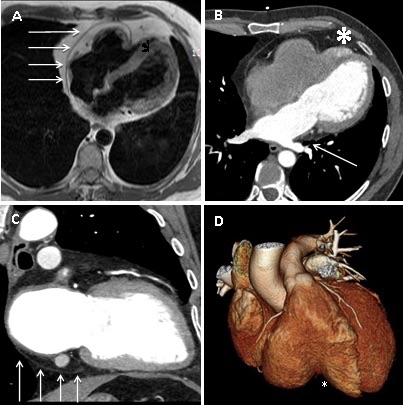
A 45 year old man presented with atrial fibrillation. A chest radiograph showed a slightly lobulated contour of the superior left heart border (see figure 1). Transthoracic echocardiography (performed at an outside institution) showed possible right ventricular (RV) mass. Cardiovascular magnetic resonance was performed to clarify the echocardiographic appearances. It demonstrated abrupt pericardial discontinuity on axial HASTE sequence, with the right-sided pericardial edge causing focal, extrinsic RV compression (Fig 2A). Steady state free precession cine images demonstrated an impaired RV ejection fraction of 34%. The RV indexed end diastolic volume was 77ml/m2 (normal age-matched range 67-111ml/m2). RV volumes quantified on short axis slices. Left ventricular (LV) morphology and function were normal (LV ejection fraction 45%). Cardiac CT was performed to provide higher spatial resolution detail of the pericardial abnormality. This was performed with retrospective gating with 20% mAs outside of diastolic reconstruction windows. This confirmed a large defect in the anterior and lateral pericardium with complete LV and partial RV herniation (Fig.2B and D). There were no discernible superior pericardial recesses (Fig. 2C) and also evidence of lung invaginating between left inferior pulmonary vein ostium and left atrium (Fig.2B, straight white line), indirectly inferring deficient pericardium in these regions. There was differential contrast opacification in the RV apex, constrained by the pericardial herniation compared to the remaining RV, implying delayed RV apical emptying but no RV apical thrombus (Fig 2B, *). No other congenital abnormality was demonstrated. The patient declined surgical pericardioplasty, accepting the risk of potential cardiac and/or vascular strangulation. The atrial fibrillation was medically managed.
Discussion:
Congenital pericardial absence is a rare condition, most frequently affecting the left-sided pericardium with either complete or partial absence and resultant LV herniation. Right-sided pericardial involvement is even less common. We present a rare case of partial absence of both left and right sides of the pericardium with complete LV herniation and partial RV herniation diagnosed non-invasively with multi-modality imaging.
Congenital pericardial absence is believed to result from pleuro-pericardial hypoxia and agenesis due to premature atrophy of the left common cardiac vein and is frequently associated with other congenital anomalies. The unusual pattern of pericardial absence and lack of concomitant congenital defect raises the possibility that the abnormality was acquired in early development, but after completion of cardiac organogenesis in this patient.
Figure 1 – PA chest radiograph. The heart appears enlarged with evidence of indentation in the superior leftward cardiac contour.
Figure 2 A. Axial HASTE image showing pericardium exerting extrinsic mass effect on the RV and apical RV herniation. B. Axial ECG-triggered cardiac CT image confirming the partial pericardial absence and demonstrating retained contrast in the herniated RV apex (*). There is lung invaginating between the left inferior pulmonary vein and left atrium (solid white arrow). C. 2-chamber reformat from ECG-gated cardiac CT showing deficient superior pericardial recesses and the inferior extent of the pericardium (solid white arrow). D. Volume-rendered ECG-triggered CT reconstruction demonstrating the point of RV partial herniation (*).
Multiple choice questions
Question 1) Congenital pericardial absence most often occurs in which geographic pattern
A- Complete absence of the pericardium
B- Absence of the left pericardium
C- Absence of the right pericardium.
Answer: B- Absence of the left pericardium. Most common defect is absence of the left pericardium (up to 70% of cases), followed by right pericardium (17%), and then total absence of the pericardium (9%).
Question 2) Of the above geographic patterns of pericardial absence, which has the best prognosis?
A- Complete absence of the pericardium
B- Absence of the left pericardium
C- Absence of the right pericardium
Answer: A- Complete absence of the pericardium. Herniation of the heart through focal pericardial defects can lead to several complications including tricuspid regurgitation, myocardial strangulation, ischaemia and sudden death. Complete absence of pericardium does not normally require intervention unless complications occur[i].
Question 3) Congenital pericardial defects result from the premature atrophy of which structure?
A- Left common cardinal vein
B- Right common cardinal vein
C- Left primitive jugular vein
D- Left vitelline vein
Answer: A- Left common cardinal vein (duct of Cuvier). As a result, reduced blood supply to the left pleuro-pericardial membrane results in pericardial agenesis[ii].
Question 4 ) Which echocardiographic finding is not typically seen in congenital partial pericardium?
A- Cardioptosis
B- Abnormal interventricular septal motion
C- Apparent right ventricular dilatation
D- Pulmonary regurgitation
Answer: D- Pulmonary regurgitation. Echocardiographic findings are related to increased cardiac mobility within the chest cavity[iii].
[i] Congenital absence of the pericardium. Hyun-Jin Kim, Young-Seok Cho et al. J Cardiovasc Ultrasound. 2014 Mar;22(1):36-39.
[ii] Congenital absence of the pericardium presenting as acute myocardial necrosis. Brulotte S, Roy L et al. Can J Cardiol. 2007 Sep; 23(11): 909-912.
[iii] Congenital absence of left pericardium. Victor AR, Osorio P et al. Rev Port Cardiol. 2003 Jun;22(6):801-10.