Will Loughborough (ST5 Radiologist), Stephen Lyen (Consultant Cardiothoracic Radiologist)
Affiliations; Bristol Royal Infirmary
Case
An 81 year old male was admitted with severe dyspnoea and hypoxia. A CT pulmonary angiogram (CTPA) was performed to identify a potential pulmonary embolus.
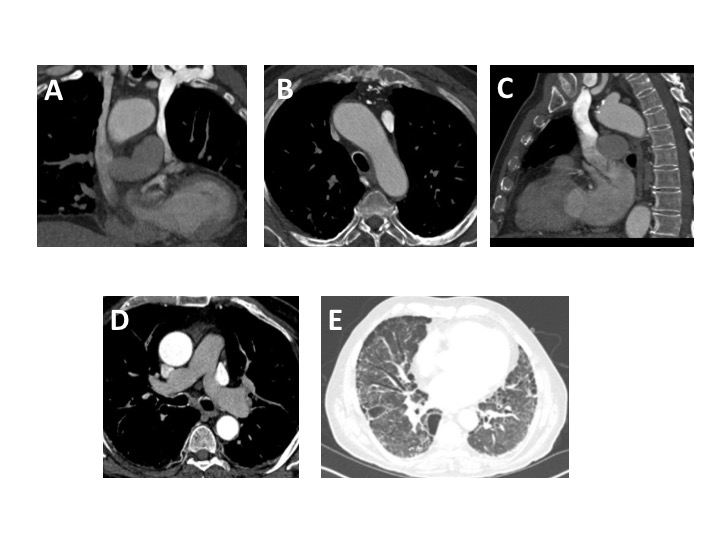
A standard protocol CTPA was performed with intravenous contrast injected via a left arm injection. A bolus tracking acquisition was used with the region of interest (ROI) centered on the main pulmonary artery (MPA). Following contrast administration, there was mild MPA opacification (below the contrast peak required for acquisition trigger). When the aorta started to opacify normally, the acquisition was manually triggered. Upon review of images, it was clear there were both right and left SVCs (figures A and B), with a small brachiocephalic venous connection. The right SVC connected to the right atrium. Unusually, the left SVC drained into the left atrium (figure C) as opposed to the coronary sinus. This explained the unusual contrast haemodynamics during study acquisition, whereby the predominant contrast flow via a left arm injection was through the left SVC into the left atrium. This is a right to left shunt, which had not resulted in any clinically significant haemodynamic consequences and indeed left atrial/ventricular size and left ventricular function were normal on echocardiography. Given this shunt, there was sub-optimal opacification of the pulmonary arteries (figure D), producing a non- diagnostic study for the detection of pulmonary emboli. A potential option would be attempting the study again with a right sided injection (with a normal drainage into the right atrium), although given the small brachiocephalic venous connection with the left SVC, there would be likely shunting of contrast and potentially, further sub-optimal MPA opacification. A ventilation/perfusion scintigraphy study was not possible due to background Usual Interstitial Pneumonitis (UIP) type pulmonary fibrosis (figure E) and centrilobular and paraseptal emphysema, which would impair results. The clinicians felt this background lung disease plus a co-existing lower respiratory tract infection explained the presenting symptoms so no further imaging was performed.
Figure Legends
Figure A. Coronal CTPA reformat – SVC duplication, with intravenous contrast delivered by left arm injection with opacification seen predominantly in the left SVC.
Figure B. Axial CTPA demonstrating greater opacification of the left-sided SVC, when compared to the right SVC
Figure C. Sagittal CTPA image through the level of the left SVC which is shown to communicate with the left atrium.
Figure D. Axial slice through the level of the MPA – non-diagnostic pulmonary arterial opacification.
Figure E – Axial slice through the lung bases on lung window settings – bronchiectasis and sub-pleural honeycombing with architectural distortion, classical for UIP-type pulmonary fibrosis.
Discussion
The most common variation to the systemic thoracic venous system is a left-sided SVC, occurring in 0.3-0.5% of the population1,2. This occurs alongside a right SVC (‘SVC duplication’) in 90% of cases, but in the remainder, a left-sided SVC occurs in isolation. In 90% cases, a left SVC connects to the coronary sinus (normal systemic venous return from the left subclavian/internal jugular veins into the right atrium)3. However, in 10% cases, as in this case, the left SVC connects directly to the left atrium 4, resulting in a right to left shunt. The presence of a left-sided SVC has a 5% association with congenital cardiac defects, most commonly an atrio-septal defect 2. A persistent left SVC results from failure of the left anterior cardinal vein to obliterate during early embryological development 2.
Whilst a left-sided SVC connected to the left atrium rarely results in haemodynamic consequences (if not associated with congenital cardiac defects), there is a risk of systemic thrombus or air embolus. Radiologically, they are important to identify as they can be mistaken for lymphadenopathy and cause confusion with central venous catheterisation 2. Additionally, as in this case, obtaining a diagnostic CTPA is challenging in SVC duplication, when the left SVC connects to the left atrium and is also connected to the right SVC.
Multiple-choice questions
Question 1:
The most common variation to the systemic thoracic venous system is;
A) SVC duplication
B) Isolated left SVC
C) Partial anomalous pulmonary venous return draining to SVC
Question 2:
A left SVC most commonly connects to;
A) Left pulmonary artery.
B) Right atrium
C) Left atrium
D) Coronary sinus
Question 3:
The most common congenital cardiac anomaly associated with a left SVC is;
A) ASD
B) VSD
C) AVSD
D) PDA
Answers 1A, 2D, 3A
References
- Pretorius PM, Gleeson FV. Case 74: right-sided superior vena cava draining into left atrium in a patient with persistent left-sided superior vena cava. Radiology. 2004 Sep;232(3):730-4.
- Burney K, Young H, Barnard SA, McCoubrie P, Darby M. CT appearances of congential and acquired abnormalities of the superior vena cava. Clinical radiology. 2007 Sep 30;62(9):837-42.
- Leibowitz AB, Halpern NA, Lee MH, Iberti TJ. Left-sided superior vena cava: a not-so-unusual vascular anomaly discovered during central venous and pulmonary artery catheterization. Critical care medicine. 1992 Aug 1;20(8):1119-22.
- Wiles HB. Two cases of left superior vena cava draining directly to a left atrium with a normal coronary sinus. Heart. 1991 Mar 1;65(3):158-60.