Authors:
Robert W. Foley, Sophie Glenn-Cox, Benjamin J. Hudson, Jonathan C. L. Rodrigues.
Affiliations:
Department of Radiology, Royal United Hospitals Bath NHS Foundation Trust, Bath, United Kingdom.
Case Report
A 36-year-old man presented to the emergency department with acute onset of severe chest pain radiating to his back. There were no high-risk exam features or a pre-existing high-risk condition. His heart rate was 40 beats per minute and regular. An urgent ECG-gated CT angiogram of the aorta was performed to exclude an acute aortic syndrome.
A retrospective spiral ECG-gated bolus-tracked acquisition (Siemens Edge, 50ml Iomeron® 350 at 5ml/sec) was performed with tube current modulation, maximum dose at 70% R-R interval and automatic best diastolic reconstruction.
The CT demonstrated a linear band of low attenuation in the ascending aorta (Figure 1).
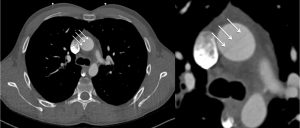 Figure 1
Figure 1
The on-call general radiologist sought a specialist opinion regarding the possibility of an aortic dissection flap. However, on review of the coronal images, the linear artefacts were repeated at regular intervals along the z-axis (Figure 2).
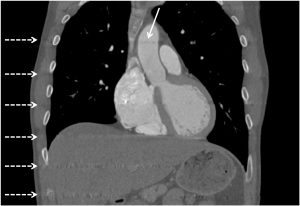
Figure 2
The original image demonstrating the linear artefact in the ascending aorta was reconstructed at 76% of the RR interval. The cardiac radiologist suspected interpolation artefact and generated additional reconstructions after ECG editing, reconstructed at 85% of the RR interval, which significantly reduced this artefact (Figure 3).
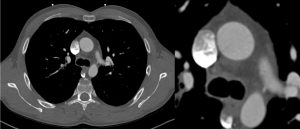
Figure 3
Data is interpolated to generative transverse reconstructions from helically acquired CT data. It assumes a photon will experience the same attenuation if it originates from any given location or 180° from that given location. However, in reality there is slice broadening, dictated by how far the CT gantry moves during a single 180° CT beam turn. Our case highlights a rare ECG-gated artefact, which also requires acquisition to be synchronised with the R-R interval. Owing to such a slow heart rate (40 beats per minute), there was insufficient data acquired during the prolonged time between R-waves and greater distance travelled by the CT gantry per heart beat in the z-axis. The regular banding artefact resulted from interpolated data between the previous and next data points acquired by the CT during consecutive R waves [1].
The benefits of ECG-gating vastly outweigh the disadvantages of non-gated techniques when acquiring CT for suspected acute aortic syndrome. However, we present a rare case of an ECG-gating specific artefact resulting from a very low heart rate. We hope that this raises the awareness of this interpolation artefact in the setting of a very low heart rate and highlights how ECG editing can help reduce the impact and thus hopefully will mitigate against potential misinterpretation, which may have important implications for the patient.
Multiple Choice Questions
- Which of the following is not considered within the spectrum of Acute Aortic Syndrome?
- Penetrating atherosclerotic ulcer
- Type A aortic dissection
- Ruptured abdominal aortic aneurysm
- Type B aortic dissection
- Intramural haematoma
- According to the BSCI/BSCCT Guidelines for CT diagnosis of acute aortic syndrome [2], which of the following is not a high risk examination feature for acute aortic syndrome?
- Systolic blood pressure deficit
- Murmur of Aortic Insufficiency
- Focal neurological deficit
- Hypertension
- Pulse Deficit
- Which of the following is not a CT artefact that could be encountered when imaging in suspected acute aortic syndrome?
- Reverberation Artefact
- Pulsation artefact
- Interpolation artefact
- Breathing artefact
- Streak artefact
- In aortic dissection, which of the following does not help differentiate the true lumen from the false lumen?
- The beak sign
- The false lumen is usually smaller
- Intraluminal thrombosis is more commonly seen in the false lumen
- The intimomedial rupture sign
- The cobweb sign
Answers
- c
- d – Hypotension, or shock, is a high-risk examination feature for acute aortic syndrome. Hypertension is a risk factor that may lead to accelerated premature degeneration of collagen and elastin within the aorta and therefore predispose to the development of acute aortic syndrome.
- a – Reverberation artefact is encountered in ultrasonography. This artefact is caused by a series of delayed echoes from a strongly reflecting interface. For example, comet-tail artefact can be encountered during echocardiography in patients with prosthetic or calcified valves.
- b – The false lumen is usually larger than the true lumen, due to increased pressure within the dissection flap. In the beak sign, there is an acute angle between the dissection flap and the outer wall of the false lumen. The intimomedial rupture sign occurs when the entry point of a dissection flap points towards the false lumen, representing the flow of blood from true lumen to false lumen. The cobweb sign is caused by thin strands of unseparated tissue between the intima and media and can be seen within the false lumen.
References
1. Kang J-W, Do K-H, Chung J-Y, Cho HJ, Seo JB, Lim T-H (2010) Concept of minimal heart rate for each pitch value to avoid interpolation artifact when using dual-source CT: a phantom study. Int J Cardiovasc Imaging 26:103–109
2. Vardhanabhuti V, Nicol E, Morgan-Hughes G, et al (2016) Recommendations for accurate CT diagnosis of suspected acute aortic syndrome (AAS)—on behalf of the British Society of Cardiovascular Imaging (BSCI)/British Society of Cardiovascular CT (BSCCT). Br J Radiol 89:20150705





