Progressive dyspnoea in a patient with a bioprosthetic AVR
Jack PM Andrews, Marc R Dweck, Alastair J Moss.
Centre for Cardiovascular Science, University of Edinburgh, Chancellor’s Building, Royal Infirmary of Edinburgh, 51 Little France Crescent, Edinburgh EH16 4TJ, UK.
Corresponding Author: Dr. Jack PM Andrews. E-mail: Jack.Andrews@ed.ac.uk
Introduction
An 85-year old woman presented to the cardiology service with exertional dyspnoea whilst walking on the flat. She underwent a bioprosthetic surgical aortic valve replacement (stentless 25 mm Kohler Elan, Vascuetec) 12 years ago for calcific aortic stenosis. She was otherwise systemically well and had not undergone any recent dental procedures. On examination, she had a collapsing pulse (BP 120/30 mmHg) and grade 3 early diastolic murmur in the aortic area. Electrocardiogram (ECG) demonstrated sinus rhythm with voltage criteria for left ventricular hypertrophy and routine bloods returned a normocytic anaemia with a mildly elevated serum bilirubin (27 umol/L). A transoesophageal echocardiogram (TOE) was performed. (Figure 1)
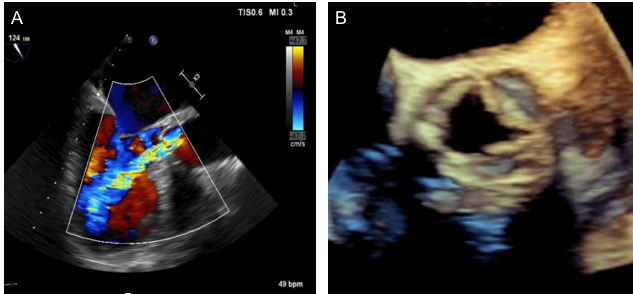
Figure 1. Transoeophageal echocardiogram mid-oesophageal AV long axis view (A). 3D echocardiogram short axis view (B).
Figure 2. Cardiac magnetic resonance demonstrated transprosthesis laminar regurgitation jet (A). 3D cardiac computed tomography coronal reconstruction of the aortic bioprosthesis confirmed the left cusp prolapse [inset] that is independent from a septated LVOT aneurysm (B). Pre TAVR deployment aortogram showing substantial volume of contrast within the left ventricle confirming significant aortic incompetence (C). Post TAVR deployment aortogram; note the lack of contrast within the left ventricle indicating the return of valvular competence and successful TAVR deployment (D).
Clinical Question
What is the aetiology of the bioprosthetic aortic valve dysfunction?
- Infective endocarditis
- Late suture dehiscence
- Leaflet prolapse
- Thrombus formation
- LVOT aneurysm formation
Answer – C
The correct answer is leaflet prolapse. TOE demonstrated a severe central regurgitant jet at the level of the prosthesis, confirmed by the large width of the colour flow jet (>65% of LVOT diameter) and colour M-mode holodiastolic flow reversal across the prosthesis (Figure 1A & B). Pathological regurgitation of prosthetic heart valves can either be central or paravalvular. Paravalvular regurgitation is often related to position of the sewing ring and anchoring tissue in the outflow tract with latent failure of the suture line due to age-related deterioration or LVOT aneurysm formation. Central regurgitation is a common feature of structural valve dysfunction. Distortions in leaflet anatomy due to perforations or thickening of the cusps ultimately result in leaflets prolapsing below the annular plane.
Whilst echocardiography remains the initial first line investigation, adjuvant imaging using cardiac magnetic resonance is increasingly utilised to confirm the severity and location of regurgitant jets (Figure 2A). [1] Bioprosthetic valve thrombosis and infective endocarditis are important differential diagnoses to exclude using modalities with superior spatial resolution such as cardiac computed tomography (Figure 2B). [2]
Figure 2C and 2D demonstrate aortograms both pre and post deployment of transcathether aortic valve replacement (TAVR) illustrating the immediate cessation of valvular incompetence. The advent of valve-in-valve interventions offers novel strategies for high-risk patients with failing stentless bioprostheses. [3] Confirming the specific aetiology of bioprosthesis dysfunction with multi-modality imaging is a priority to select the most appropriate therapeutic strategy. This patient underwent transcatheter aortic valve implantation (26mm CoreValve Evolut R, Medtronic) with an immediate improvement in symptoms.
REFERENCES
[1] Salaun E, Jacquier A, Theron A, Giorgi R, Lambert M, Jaussaud N, Hubert S, Collart F, Bonnet JL, Habib G, Cuisset T, Grisoli D. Value of CMR in quantification of paravalvular aortic regurgitation after TAVI. Eur Heart J – Cardiovascular Imaging. 2016;17:41-50.
[2] Moss AJ, Dweck MR, Dreisbach JG, Williams MC, Mak SM, Cartlidge T, Nicol ED, Morgan-Hughes GJ. Complementary role of cardiac CT in the assessment of aortic valve replacement dysfunction. Open Heart. 2016;3:e000494. Doi: 10.1136/openhrt-2016-000494.
[3] Duncan A, Davies S, Di Mario C, Moat N. Valve-in-valve transcatheter aortic valve implantation for failing surgical aortic stentless bioprosthetic valves: A single-center experience. J Thorac Cardiovasc Surg. 2015;150:91-98.