Dr Jonathan Rodrigues, Bristol Heart Institute
Case:
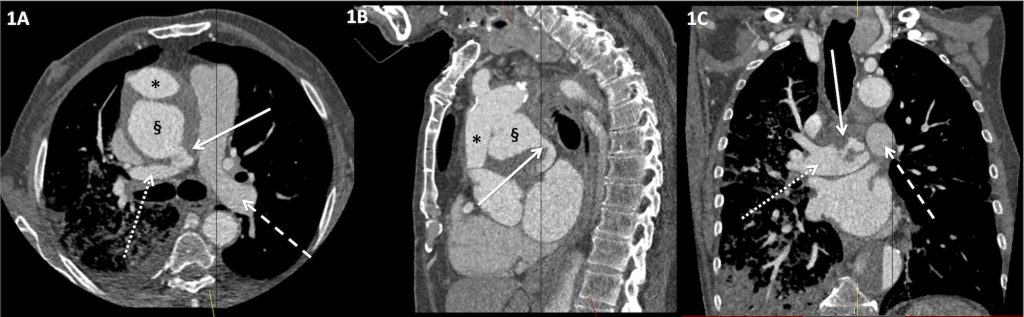
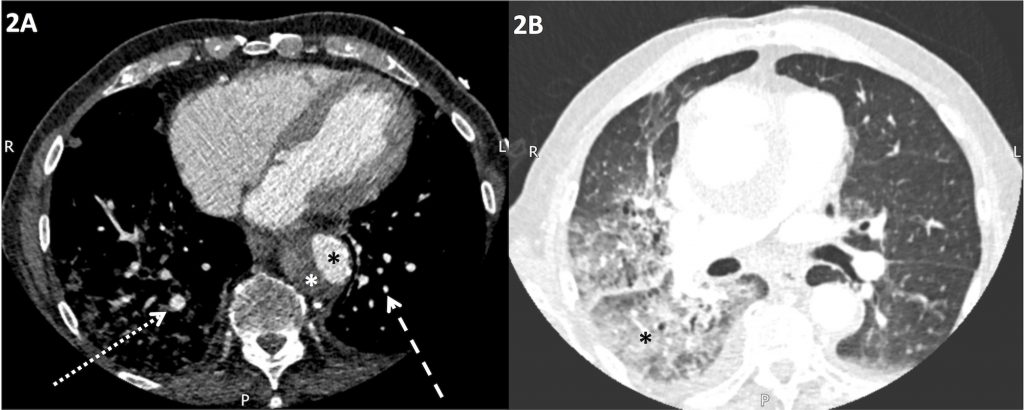
An elderly gentleman presented with chest pain, shortness of breath and haemoptysis. His past medical history was significant for previous type A aortic dissection and ascending aortic repair many years ago. On examination, he was hypoxic and cyanosed. An urgent, non-ECG gated CT aorta was performed. This revealed a large pseudoaneurysm arising from the superior aspect of the ascending aortic repair (Figure 1A and 1B). The pseudoaneurysm was in direct continuity with the right main pulmonary artery (Figure 1A-C). There was evidence of significant left to right shunt from ascending aorta, via the pseudoaneurysm, into the right-sided pulmonary arterial system, with differential opacification of the main pulmonary arteries, with avid right-sided enhancement on the systemic arterial phase study (Figure 1A and 1C). The discrepancy in size of segmental and subsegmental pulmonary arteries, larger in the right lower lobe compared to the left, was suggestive of acute right-sided pulmonary arterial volume loading (Figure 2A). The airspace opacification in the middle and right lower lobes (Figure 2B) was consistent with alveolar oedema and possibly haemorrhage from rapid significantly increased hydrostatic pressure and possibility capillary haemorrhage due to the large volume acute shunt. Unfortunately, the patient deteriorated very quickly and did not survive for definitive surgical correction to be attempted.
Discussion:
Acquired aorto-pulmonary artery fistulation is a rare but life-threatening condition. It may arise as a complication of aortic aneurysms[1] and both acute and chronic aortic dissections[2]. However, progression of a post-aortic surgery pseudoaneurym to an acquired aorto-pulmonary fistula is exceedingly rare. Potential causes for such a rare complication are postulated to include longstanding right pulmonary arterial compression by the pseudoaneurysm, atherosclerosis, connective tissue disorders, necrosis, trauma, inflammatory aortitis and infection [3]. Aorto-pulmonary fistulae can be asymptomatic [4] or more commonly present with congestive heart failure, chest pain and haemoptysis [5]. Definitive treatment of aorto-pulmonary fistulae is usually surgery. However, treatment with Amplatzer Septal Occluder has previous been described [6].
Figure 1. Non-ECG gated arterial phase CT of the thorax.
A) Axial image showing a large ascending aortic pseudoaneurysm (§) exerting mass effect on the ascending aortic graft repair (*), from previous type A aortic dissection. There is a direct connection between the ascending aortic pseudoaneurysm and the right main pulmonary artery (solid white arrow). There is differential opacification of the right and left main pulmonary arteries with more avid enhancement in the right main pulmonary artery (dotted white arrow) compared to the left main pulmonary artery (dashed white arrow) on this arterial phase study.
B) Sagittal reformatted image showing the ascending aortic graft repair (*) with large pseudoaneurysm arising from the proximal aspect of the graft repair (§). The connection between the pseudoaneurysm and the right main pulmonary artery is demonstrated (solid white arrow).
C) Coronal reformatted image showing an abnormal serpiginous connection with the right main pulmonary artery (solid white arrow) and differential opacification of the main pulmonary arteries on this systemic arterial phase study, with more avid opacification of the right main pulmonary artery (dotted white arrow) compared to the left main pulmonary artery (dashed white arrow).
Figure 2. Non-ECG gated arterial phase CT of the thorax
A) Axial image display on mediastinal window settings showing asymmetrical enlargement of the right basal segmental and subsegmental pulmonary arteries (dotted white arrow) compared to the left basal pulmonary arteries (dashed white arrow). There is evidence of previous dissection in the descending thoracic aorta with opacified oval-shaped true lumen (black *) and thrombosed false lumen (white *).
B) Axial image displayed on lung window settings showing focal consolidation in the right lower lobe (*) and the lateral segment of the middle lobe. In this clinical context, this was consistent with alveolar haemorrhage.
References
[1] Boyd LJ. A study of four thousand reported cases of aneurysm of the thoracic aorta. Am J Med Sci. 1924; 168: 654-663.
[2] Piciche M, De Paulis R, Chiariello L. A review of aortopulmonary fistulas in aortic dissection. Ann Thorac Surg. 1999; 68: 1833-6.
[3] Mukadam M, Barraclough J, Riley P, et al. Acquired aorto-pulmonary artery fistula following proximal aortic surgery. Interact Cardiovasc Thorac Surg. 2005; 4: 388-90.
[3] Maeder MT, Wobler T, Kunzli A et al. Aortopulmonary fistula occurring 4 years after replacement of the ascending aorta. Ann Thorac Surg. 2006; 81: e18-e20.
[4] Ferrari G, Anastasio G, Bianchi M et al. Aortopulmonary fistula after a modified bentall procedure. J Heart Valve Dis. 2012; 21: 505-508.
[5] Wakefield BJ, Winter D, Alfirevic A. Staged repair of an aortopulmonary fistula from a large ascending aortic pseudoaneurysm: the role of transesophageal echocardiography. J Cardiothorac Vasc Anesth. 2015. doi: 10.1053/j.jvca.2015.11.022. [Epub ahead of print].
[6] Coserria F, Mendez A, Moruno A, et al. Percutaneous closure of iatrogenic aortopulmonary fistula using the Amplatzer Septal Occluder. Rev Esp Cardiol. 2014: 67: 228-229.