Single narrow left sided stenotic pulmonary vein leading to pleural effusion and pulmonary congestion
Vicky Tilliridou, Michelle C Williams.
Royal Infirmary of Edinburgh, Edinburgh, United Kingdom.
Case Report
A 42-year-old gentleman with paroxysmal atrial fibrillation underwent multiple electrophysiological interventions for symptoms refractory to medication. These included several radiofrequency ablations and one cryoablation for pulmonary vein isolation. Three weeks post-cryoablation, he reported right-sided non-exertional chest pains lasting for up to 5 minutes per episode with associated chronic cough and exertional breathlessness.
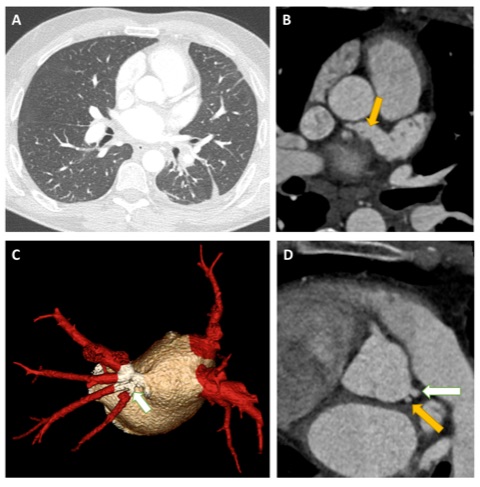
Computed tomography coronary angiography (CTCA) was performed to evaluate the pulmonary venous anatomy. Four pulmonary veins were visualised draining together into the left atrium with stenosis of the left lower pulmonary vein. Wide field-of-view images demonstrated features of pulmonary venous congestion and a small left pleural effusion. Additionally a large, patent “chicken wing” atrial appendage was present. Incidentally, the left coronary artery had separate origins from the left coronary cups for the left anterior descending artery and left circumflex artery.
Figure: A. Wide field-of-view image showing evidence of cardiac failure (increased fluid in the fissures) and a left pleural effusion. B. Axial image showing a very large left atrial appendage with a “chicken wing” configuration (yellow arrow). C. 3D reconstruction showing two pulmonary veins on the right and one pulmonary vein on the left with a stenotic narrowing at the ostium. D. Separate origins of the left anterior descending and left circumflex artery from the left coronary cusp.
Discussion
Radiofrequency catheter ablation was introduced in the 1980s as a novel treatment method for atrial fibrillation. It was initially performed within the pulmonary vein itself but this commonly led to pulmonary vein stenosis. The technique evolved to performing circumferential ablation in the cardiac antrum around the ostia of the pulmonary veins has become the standard approach with a reduced long-term risk of pulmonary vein stenosis (1). In the most widely used definition, from the HRS/EHRA/ECAS Expert Consensus Statement, mild stenosis is present if the reduction compared to pre-ablation diameter is < 50%, moderate if 50-70%, and severe if ≥ 70% (2). Recent data shows that acquired pulmonary veins stenosis secondary to catheter ablation for atrial fibrillation occurs in a mean of 2% and a median of 3.1% of cases (3). However, the incidence following ablation for atrial fibrillation may be underestimated as patients may be asymptomatic or may remain unrecognised due to non-specific symptoms. Indeed, although symptoms may include chest pain, breathlessness, cough, or haemoptysis, patients often remain asymptomatic if the collateral circulation compensates for the reduced flow through the narrowed pulmonary vein(s).
Plain radiography and CT imaging may show pulmonary venous congestion or pleural effusions, however these are non-specific signs of left-sided heart failure. Diagnosis of pulmonary vein stenosis can be achieved with CT angiography, magnetic resonance imaging, transoesophageal echocardiography or catheter venography (4-6).
Multiple choice questions
1. In what proportion of the population is the typical pattern of four pulmonary veins and four well-differentiated ostia seen? (7)
A) <50%
B) 60-70%
C) 70-80%
D) 80-90%
E) >90%
2. Which is the most common focus of atrial fibrillation? (7)
A) Left superior pulmonary vein
B) Left inferior pulmonary vein
C) Right superior pulmonary vein
D) Right inferior pulmonary vein
3. Which imaging modality can identify and quantify pulmonary vein stenosis?
A) Plain radiography
B) CT angiography
C) MR perfusion
D) Single photon emission tomography
Answers
1 = B
2 = A
3 = B
References
1. Edriss H, Denega T, Test V, Nugent K. Pulmonary vein stenosis complicating radiofrequency catheter ablation for atrial fibrillation: A literature review. Respir Med. 2016;117:215-22.
2. Calkins H, Kuck KH, Cappato R, Brugada J, Camm AJ, Chen SA, et al. 2012 HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012;14(4):528-606.
3. Pazos-Lopez P, Garcia-Rodriguez C, Guitian-Gonzalez A, Paredes-Galan E, Alvarez-Moure MA, Rodriguez-Alvarez M, et al. Pulmonary vein stenosis: Etiology, diagnosis and management. World J Cardiol. 2016;8(1):81-8.
4. Schneider C, Ernst S, Bahlmann E, Malisius R, Krumsdorf U, Boczor S, et al. Transesophageal echocardiography: a screening method for pulmonary vein stenosis after catheter ablation of atrial fibrillation. Eur J Echocardiogr. 2006;7(6):447-56.
5. Scharf C, Sneider M, Case I, Chugh A, Lai SW, Pelosi F, Jr., et al. Anatomy of the pulmonary veins in patients with atrial fibrillation and effects of segmental ostial ablation analyzed by computed tomography. J Cardiovasc Electrophysiol. 2003;14(2):150-5.
6. Yang M, Akbari H, Reddy GP, Higgins CB. Identification of pulmonary vein stenosis after radiofrequency ablation for atrial fibrillation using MRI. J Comput Assist Tomogr. 2001;25(1):34-5.
7. Porres DV, Morenza OP, Pallisa E, Roque A, Andreu J, Martinez M. Learning from the pulmonary veins. Radiographics. 2013;33(4):999-1022.