A Complicated Infarct
I Harries1, B Berlot1, R Ascione2, M Hamilton3, C Bucciarelli-Ducci1
1. Department of Cardiology, Bristol Heart Institute, United Kingdom
2. Department of Cardiothoracic Surgery, Bristol Heart Institute, United Kingdom
3. Department of Radiology, Bristol Royal Infirmary, United Kingdom
A 53 year old male ex-smoker with no other cardiovascular risk factors presented to a local hospital with progressive dyspnoea following an episode of chest pain that had occurred six weeks prior. ECG showed sinus rhythm with anterior Q waves. Coronary angiography demonstrated a proximal occlusion of the left anterior descending (LAD) artery and mild non-flow limiting disease in the right and left circumflex coronary arteries. The patient was commenced on appropriate medical therapy and transferred to our institution for cardiac magnetic resonance (CMR) imaging to evaluate LAD territory viability.
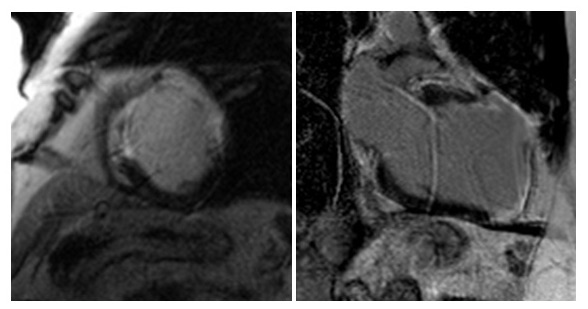
Figure 1. Mid ventricular short and 2 chamber long axis PSIR late Gadolinium enhancement sequences of the left ventricle.
- Is the LAD territory viable?
- No
- Yes
Answer:
- No. The LAD territory is not viable. There is transmural late enhancement of the mid antero-septal, mid-anterior and mid anterolateral walls on the short axis view, and of the mid and apical anterior walls and apical cap on the long axis (2 chamber) view. The likelihood of functional recovery following revascularisation is very low in segments with >75% hyperenhancement 1.
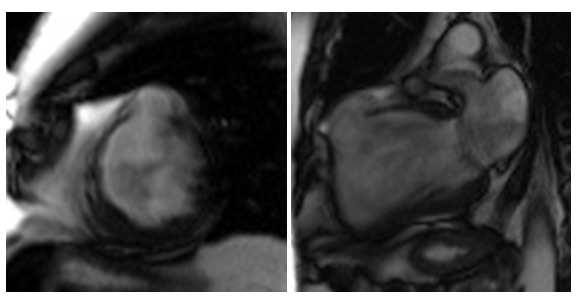
Figure 2. Mid ventricular short axis and long axis 2 chamber balanced SSFP cine stills of the left ventricle.
- What complication of myocardial infarction is demonstrated?
- Left ventricular aneurysm
- Ventricular septal defect
- Papillary muscle rupture
- Left ventricular pseudoaneurysm
- Left ventricular thrombus
Answer:
d. Left ventricular pseudoaneurysm. Myocardial rupture is evidenced by the abrupt discontinuation of the myocardium in the mid anterior segment (white arrow) with containment by the overlying pericardium (red arrow).
Figure 3. Zoomed mid ventricular short axis balanced SSFP cine still of the left ventricle.
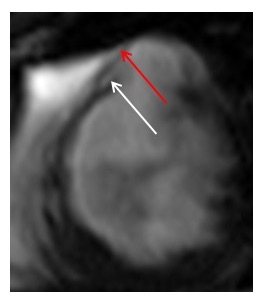
A pseudoaneurysm or ‘false aneurysm’ is formed when cardiac rupture is contained by adherent pericardium or scar tissue. Unlike true aneurysms, pseudoaneurysms contain no endocardium or myocardium and are significantly more likely to rupture than true aneurysms, which rarely rupture because of the densely fibrotic tissue found in the wall of true aneurysms 2.
- What is the appropriate management strategy?
- Surgical repair
- Medical therapy
- Revascularisation of the LAD (CABG or PCI)
- Cardiac transplant
Answer:
- Surgical repair. If feasible, surgical repair is the preferred therapeutic option because conservative management of pseudoaneurysms carries a 30-45% risk of rupture and a mortality of almost 50%3. Perioperative mortality is less than 10% with greater risk for patients requiring concomitant mitral valve repair2.
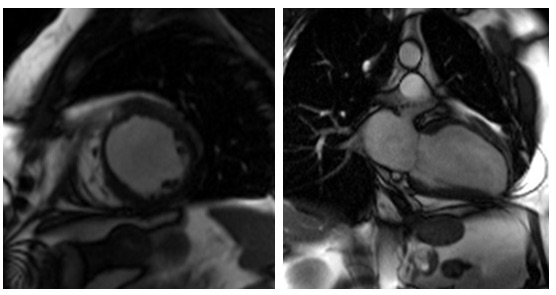
The patient successfully underwent left ventricular aneurysmectomy (Figure 4.), was established on appropriate medical therapy, had a primary prevention ICD implanted and is making a good recovery.
Figure 4. Mid ventricular short axis and long axis 2 chamber balanced SSFP cine stills of the left ventricle following left ventricular aneurysmectomy.
References
- Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000 Nov 16;343(20):1445-53.
- Shapira O. (2017, Nov 27) Left ventricular aneurysm and pseudoaneurysm following acute myocardial infarction. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4900369/.
- Frances C, Romero A, Grady D. Left ventricular pseudoaneurysm. J Am Coll Cardiol. 1998 Sep;32(3):557-61.





