Mr Dilliram Adhikari1, Mrs Vimbai Tungwarara1, Dr Badrinathan Chandrasekaran2, Professor Stefan Neubauer1, Dr Chrysovalantou Nikolaidou1
- Oxford Centre for Clinical Magnetic Resonance Research, University of Oxford, Oxford
- Wiltshire Cardiac Center, Great Western Hospital, Swindon
Case history
A 82-year-old man, with previous history of bypass surgery (left internal mammary artery to left anterior descending artery, and saphenous venous grafts to obtuse marginal and posterior descending artey) in 2014, was referred for a cardiac magnetic resonance (CMR) scan to further characterise a large pericardial mass seen on echocardiogram (Image 1), which was performed due to newly diagnosed heart failure. Cardiac catheterisation showed patent bypass grafts, and no evidence of pericardial constriction.
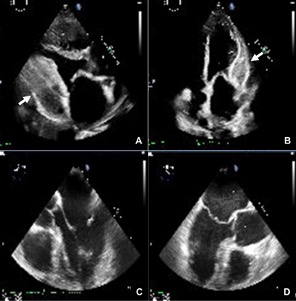
Image 1. Transthoracic echocardiogram showing a large pericardial mass on the parasternal long-axis (A) and apical 4-chamber views (B) (arrows). No evidence of the mass on a transoesophageal echocardiogram from May 2017 (C, D).
The CMR was performed on a 1.5T Magnetom Avanto-Fit (Siemens, Erlangen, Germany) scanner, using a dedicated protocol for cardiac masses, including cine imaging, tissue characterisation with T1- and T2-weighted imaging and parametric mapping, fat suppression, early and late gadolinium imaging, and rest perfusion imaging. CMR revealed a large, elongated mass (95mm in length x 29 mm in width) within the pericardial space, adjacent to the basal-mid lateral and inferior and the apical inferior left ventricular wall. The mass was well circumscribed with smooth margins and had slightly heterogeneous signal intensity. It did not appear to cross tissue planes and there was no evidence of invasion to the myocardium or extracardiac structures, or compression of the left ventricle. There was no significant pericardial effusion. The mass appeared largely avascular on rest perfusion, early gadolinium enhancement, and late gadolinium enhancement. On late gadolinium imaging, most of the mass showed no enhancement, however, there were small areas of enhancement within the mass and enhancement of its margins (possible fibrous tissue) (Image 2). It had higher signal intensity compared to the myocardium on T1-weighted imaging and T2-weighted imaging and did not demonstrate fat-suppression. Native myocardial T1 values were overall low on T1-mapping (less than 700 ms; normal ShMOLLI myocardial T1 range, 941±23 ms), with pockets of significantly elevated T1 values, while T2 values were significantly elevated on T2-mapping (T2 up to 83 ms; normal myocardial T2 range 48±2 ms at 1.5T in our centre), suggestive of fluid within the mass (Image 3). There was moderate biventricular dilatation and mild biventricular systolic dysfunction, with a moderate-sized myocardial infarction (50-75% wall thickness) in the lateral left ventricular wall.
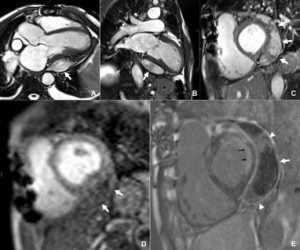
Image 2. Left ventricular outflow tract (A), vertical long-axis (B) and mid-ventricular short-axis (C) still frames from cine steady-state free precession (SSFP) imaging, showing the large well-circumscribed mass around the lateral and inferior left ventricular wall (arrows). The mass demonstrates minimal contrast uptake on first-pass perfusion imaging (D), only small pockets of enhancement (arrowheads) within the mass and enhancement of its margins (arrow) on free-breathing motion-corrected late gadolinium imaging (E). The black arrows show a previous lateral myocardial infarction.
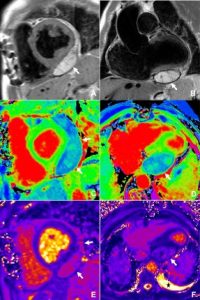
Image 3. Tissue characterisation of the pericardial mass. Mid-ventricular short-axis T1-weighted image (A) and coronal left ventricular outflow tract T2-weighted image (B) showing the well-demarcated mass with smooth margins, and higher signal intensity compared to the myocardium. T1-mapping short-axis (C) and horizontal long-axis (D) views demonstrating low T1 values of the mass compared to the myocardium. Respective views of the heart on T2-mapping demonstrate high T2 values within the mass. The asterisk shows the small pericardial effusion.
Overall, the findings were in keeping with a benign lesion, which, based on the imaging characteristics, most likely represented organised thrombus/haematoma. A differential diagnosis of secondary or primary cardiac tumour was considered less likely in the absence of invasion across tissue planes and vascular perfusion. The patient denied any history of trauma. Given the absence of compression of cardiac chambers or adjacent structures on CMR and the absence of constrictive physiology on cardiac catheterisation, a conservative management with follow-up imaging was decided. The patient is feeling better on heart failure treatment.
Questions
- What are the imaging characteristics of a pericardial cyst on CMR?
- They are most commonly seen in the right cardiophrenic angle
- They have low to intermediate signal intensity on T1-weighted imaging, and high signal intensity on T2-weighted imaging
- They typically enhance after gadolinium administration
- They are associated with large pericardial effusion
Answers: A, B
- Describe common non-neoplastic pericardial lesions
Answers: pericardial cyst, pericardial diverticula, pericardial haematoma
- Which are the CMR tissue characteristics of a pericardial haematoma?
- Heterogenous signal intensity, with areas of high T1 and T2 during the subacute phase
- Heterogenous signal intensity, with areas of low T1 and high T2 during the subacute phase
- Increase in T1 and T2 signal intensity in the chronic phase
- Decrease in T1 and T2 signal intensity in the chronic phase
Answers: A, D
Discussion
The normal pericardium consists of two layers, the serous and fibrous pericardium, which appear as a smooth, thin (less than 2 mm), low-intensity curvilinear structure on cine CMR imaging. The pericardial cavity is a small space, which normally contains between 10 and 50 ml of ultrafiltrate of plasma, and appears as a small rim of fluid around the heart (1). Although pericardial diseases, such as pericarditis or pericardial effusion, are fairly common, pericardial masses are rare, with a prevalence of primary pericardial neoplasms from about 0.001 to 0.007% (2). Pericardial masses can be divided into neoplastic, primary and secondary, and non-neoplastic. The most common benign lesions are pericardial cysts and lipomas. Malignant pericardial masses include mesothelioma, sarcoma, lymphoma and metastatic tumours from the breast, lung and bone marrow (3).
Haemopericardium usually presents acutely after trauma with haemodynamic compromise, however, rare cases of late presentation and progression to constrictive pericarditis and subsequent heart failure have been described. Compared to simple pericardial cysts, haemopericardium is characterised by a heterogeneous high-signal intensity on T1 and T2-weighted CMR imaging in the subacute phase. In the chronic phase, haematomas have a thick rim from hemosiderin deposition and internal foci of varying intensity from calcification, fibrosis, or hemosiderin deposition, the latter resulting in lower signal intensity on native T1 and T2-mapping (4).
CMR can provide information on the size and location of pericardial masses, their extension and relationship to adjacent structures, allowing for assessment of feasibility for surgical resection. Although pathology remains the gold standard for the accurate diagnosis of the type of a mass, CMR can provide crucial non-invasive information on tissue characterisation, and aid the differential diagnosis. CMR can also provide information about pericardial inflammation, adhesions to the myocardium, and evidence of constrictive physiology. In our case, it provided the diagnosis of a benign lesion, most likely pericardial haematoma/thrombus, with no compression of the cardiac chambers, thus helped avoid a re-sternotomy for biopsy of the mass.
References
- Bogaert J, Francone M. Cardiovascular magnetic resonance in pericardial diseases. J Cardiovasc Magn Reson. 2009;11(1):14.
- Restrepo CS, Vargas D, Ocazionez D, Martínez-Jiménez S, Cuellar SLB, Gutierrez FR. Primary Pericardial Tumors. RadioGraphics. 2013;33(6):1613-30.
- Tower-Rader A, Kwon D. Pericardial Masses, Cysts and Diverticula: A Comprehensive Review Using Multimodality Imaging. Prog Cardiovasc Dis. 2017;59(4):389-97.
- Watson WD, Ferreira VM, Sayeed R, Rider OJ. Serial Cardiac Magnetic Resonance of an Evolving Subacute Pericardial Hematoma. Circulation: Cardiovascular Imaging. 2019;12(12):e009753.





