Recurrent haemoptysis – but why?
Dr Jonathan Weir-McCall, University of Dundee.
Case History
A 59 year old female presented to clinic with a history of recurrent haemoptysis. This had first occurred 14 years ago, with this being the 4th episode since that first occurrence. Each time, the haemoptysis occurred without a prodrome and resulted in about half a cupful of fresh blood being produced. She stopped smoking 2 years ago, prior to which she had a 30 pack year history. She is otherwise fit and well. The GP had performed FBC, U&Es, LFTs, CRP and a CXR prior to referral, all of which were normal.
Questions
Q1. Given the history and initial test results, which of the following is the most likely differential diagnosis?
- Chronic bronchitis
- Chronic thromboembolic pulmonary emboli
- Pulmonary AVM
- Bronchial carcinoma
The differential diagnosis for haemoptysis is wide, however has been somewhat narrowed down by the 14 year intermittent history, normal blood results and normal chest x-ray.
In a recent smoker, bronchiectasis and chronic bronchitis are the most common causes of haemoptysis.1 Given the intermittent nature of the bleeding, a small AVM should be considered. Vasculitis should also be in the differential although this is unlikely with no shortness of breath, and normal bloods. While malignancy is always in the differential for a recent smoker presenting with haemoptysis this would be unusual given the 14 year history. Given this range of differentials an ECG-gated pulmonary angiogram was performed.
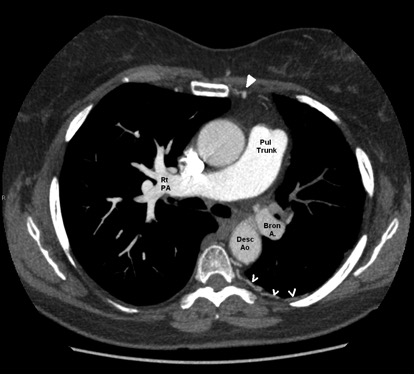
Fig 1: ECG-gated pulmonary angiogram:
Q2. What does the CT image in Figure 1 show?
- Bronchopulmonary sequestration
- Chronic pulmonary thromboembolism
- Anomalous pulmonary venous drainage
- Unilateral absence of a pulmonary artery
The CT image is an axial slice of the thorax from a CT pulmonary angiogram study as evidenced by the dense enhancement of the pulmonary artery.
The right pulmonary artery courses in direct continuity from the pulmonary trunk, however the left pulmonary artery is not seen connecting with the pulmonary trunk. In addition to this, the vessel in the region of the left pulmonary artery is poorly enhanced compared with the right pulmonary artery, and matches the enhancement seen in the descending aorta. The combination of these features is in keeping with isolated unilateral absence of the pulmonary artery (IUAPA)2 with compensatory dilatation of the bronchial artery arising from the descending aorta. As well as the dilated bronchial artery, the left internal mammary artery and intercostal arteries are also dilated, acting as further sources of collateral supply to the left lung. The left lung is small compared with the right due to a degree of pulmonary atresia (Figure 2).
Figure 2: Annotated figure demonstrating the variant anatomy of this case of Isolated unilateral absence of a pulmonary artery

Pul Trunk = Pulmonary trunk, Rt PAS = right pulmonary artery, Desc Ao = descending aorta, Bron A = Bronchial artery. Filled in arrowhead points to a dilated Left internal mammary artery (cf the other side), Open arrows point to dilated intercostal arteries.
Q3: What complications is this patient at risk of?
- Left-sided pulmonary hypertension
- Right sided bronchiectasis
- Left sided haemoptysis
- Pulmonary embolism
Recurrent infections, dyspnoea and decreased exercise tolerance are the most common presentations of this condition.2 In addition to this there are several important sequalae. Due to the increased blood through the single remaining pulmonary artery these patients are at high risk for developing pulmonary artery hypertension, this is especially pronounced during pregnancy, and indeed this can be the trigger that leads to the condition being discovered.4 Reduced blood supply to the side with the absent pulmonary artery predisposes it to recurrent infections with reports of bronchiectasis secondary to this.3 The dilated bronchial artery, internal mammary arteries and intercostal arteries are all at increased risk of bleeding due to the increased pressures running through them and their abnormal tortuous nature. Patients with IUAPA are also at increased risk for high altitude pulmonary oedema and should be warned as such. UAPA can occur with other congenital anomalies (in which case it is no longer “isolated”), in particular ASDs, VSDs and Tetralogy of Fallot. Echocardiography is a useful adjunct in investigation as it can assess for these at the same time as measuring for pulmonary artery pressures to diagnose pulmonary hypertension.
References:
- Tsoumakidou M, Chrysofakis G, Tsiligianni I, Maltezakis G, Siafakas NM, Tzanakis N. A prospective analysis of 184 hemoptysis cases: diagnostic impact of chest X-ray, computed tomography, bronchoscopy. Respiration. 2006;73(6):808-14. Epub 2006 Jan 27.
- Ten Harkel AD, Blom NA, Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest. 2002 Oct;122(4):1471-7.
- Yiu MWC, Le DV, Leung Y, Ooi CGC. Radiological features of isolated unilateral absence of the pulmonary artery. J HK Coll Radiol 2001;4:277-280.
- Stiller RJ, Soberman S, Turetsky A, et al. Agenesis of the pulmonary artery,: an unusual cause of dyspnea in pregnancy. Am J Obstet Gynecol 1988; 158:172-173.