Authors: Dr Bronagh P Kelly, Dr Christopher J Lockhart, Dr Mark S Spence, Dr C Owens
Department of Adult Congenital Heart Disease, Belfast Heart Centre, Royal Victoria Hospital, Belfast
Case History:
A 76 year old female presented to the emergency department with hypoxic respiratory failure. She had recently commenced first round of chemotherapy for squamous cell lung cancer and 3 months prior to presentation patient had underwent a right lower lobectomy. Other history included ulcerative colitis, raynaud’s and polymyalgia rheumatica.
Due to increasing oxygen requirements and the need for AIRVO the patient was transferred to the intensive care unit (ICU). Computed tomography pulmonary angiogram (CTPA) demonstrated no evidence of pulmonary embolism/consolidation.
Whilst in ICU, it was observed that saturations improved in the supine position; SaO2 when lying supine was 96% on 4 litres and fell rapidly to 84% on sitting up with the same oxygen administration.
Transthoracic echocardiogram demonstrated a Secundum Atrial Septal Defect.
Bubble echo and transoesophageal echocardiogram demonstrated marked channelling of right atrial flow across a small ASD, demonstrating right to left flow.
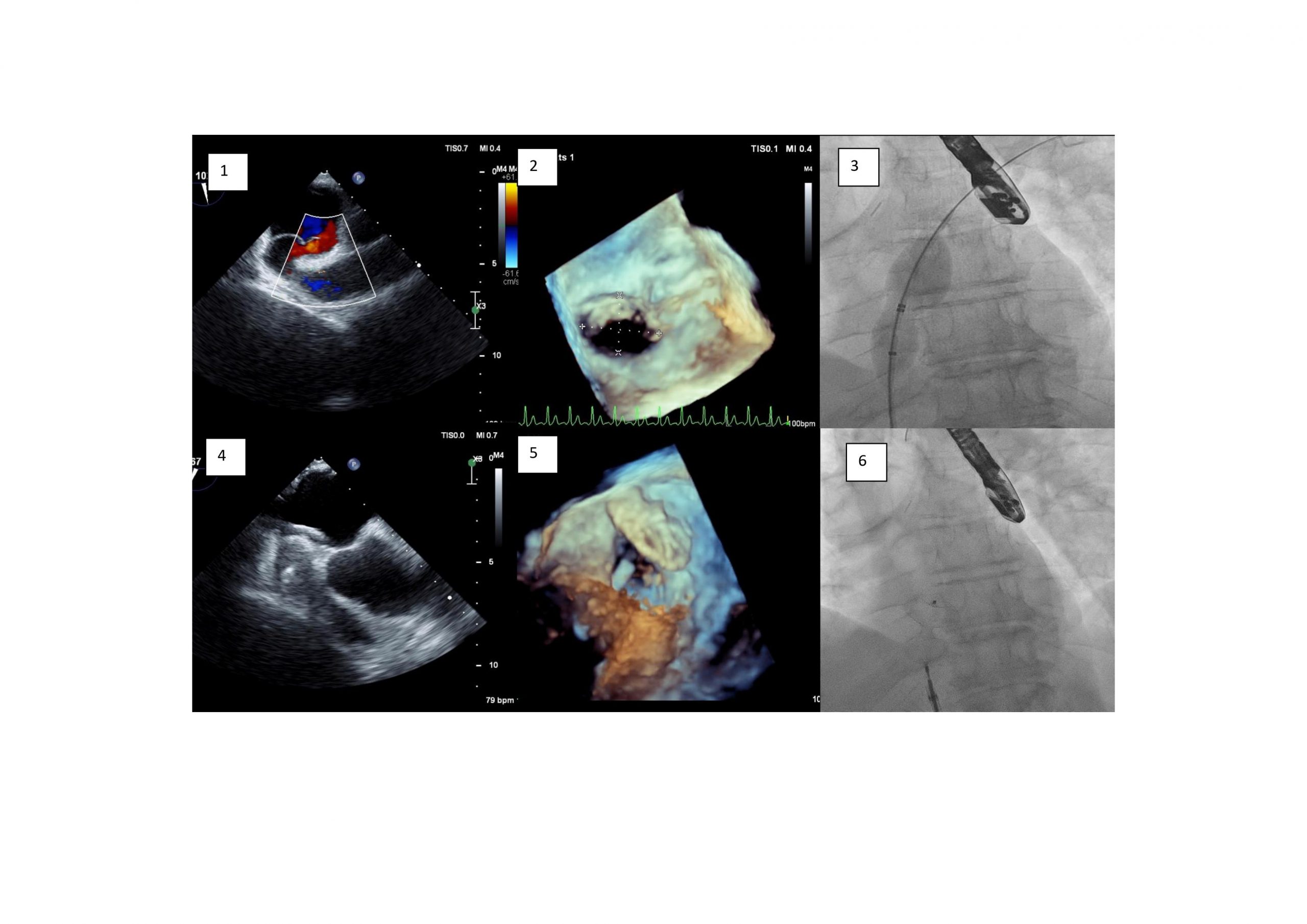
The patient proceeded to catheter closure of atrial septal defect using transoesophageal guidance. A sizing balloon was used to occlude the ASD. Saturations rose to 99%. Subsequently a 14 mm Amplatzer septal occluder was deployed using a 9F Torqvue. This resulted in an improvement in the patient’s saturations eliminating the need for additional oxygen supplementation.
Questions
1 . In the presence of an intraatrial communication, what factors precipitate platypnea orthodeoxia syndrome?
- intracardiac shunting
- pulmonary shunting
- ventilation-perfusion mismatch
- all of the above
Answer: D
2. Which of the following statements are true with regards to indication and method of ASD closure?
- An ASD should be closed if there is right ventricular volume overload in the absence of evidence of pulmonary hypertension or left ventricle dysfunction
- Surgical closure is the 1st line method for closure of a secundum ASD
- Percutaneous device closure is 1st line method of closure of secundum ASD when technically feasible
- ASD closure should be considered in patients with suspicion of paradoxical embolism (exclusion of other causes), providing there is absence of PAH and LV disease.
- ASD closure is recommended in patients with Eisenmenger physiology.
Answer:
True: A, C, D
False: B, E (Percutaneous device closure is recommended as method of choice for secundim ASD when technically suitable, ASD closure is NOT recommended in patient’s with Eisenmenger physiology)
3. POS can occur in the presence of intra-atrial shunting either via an ASD or patient foramen ovale (PFO). What are the other indications to close a PFO?
- CVA or TIA in patients over the age of 65 in whom paradoxical embolism through patent foramen ovale is considered to be the cause
- Migraines
- Decompression diving illness
- Increased right ventricular volume overload
- CVA or TIA in patients under the age of 65 in whom paradoxical embolism through patent foramen ovale is considered to be the cause
Answer: C and E
European Consensus paper 2018 “Perform percutaneous closure of a PFO in carefully selected patients aged from 18 to 65 years with a confirmed cryptogenic stroke, TIA, or systemic embolism and an estimated high probability of a causal role of the PFO as assessed by clinical, anatomical and imaging features” (!)
Decompression diving illness is an indication for PFO closure for high volume divers who wish to continue diving (“). There is insufficient evidence to recommend PFO closure for the indication of migraine.
Discussion:
Platypnoea Orthodeoxia Syndrome (POS) is a rare, undiagnosed, positional dependent phenomenon characterised by hypoxaemia and dyspnoea improves on supine positioning.1
Diagnostic work-up of POS includes transoesophageal echocardiography (TOE) to interrogate for a right to left intracardiac shunt via a patent foramen ovale (PFO) or atrial septal defect (ASD).2
The three main subsets of POS are caused by; intracardiac shunt, pulmonary arteriovenous shunts (eg hepatopulmonary syndrome, hereditary haemorrhagic telangiectasia) or ventilation/perfusions mismatch in the lungs (eg emphysema/COPD, autonomic dysfunction). 3
The pathogenesis of right-to-left atrial shunting with normal intracardiac pressures persists as an area of discussion 4. The median age of patients with POS is in the 7th decade 3
Interatrial right to left shunting is anticipated in the setting of elevated pulmonary pressures, however in cardiac POS, these pressures are usually normal 5. Therefore, it appears that both an anatomic and a functional component are both required for this shunting to occur, the functional component facilitating the shunting of deoxygenated blood and cause an inverted direction of flow with orthostatism. 3 Although this is not fully understood.
Debilitating dyspnoea secondary to POS can be successfully relieved by closure of the inter-atrial communication6.
Symptomatic improvement is seen in >95% of patients treated with percutaneous closure 5.
References:
- Knapper, J, Schultz, J. Cardiac Platypnea-Orthodeoxia Syndrome: An Often Unrecognised Malady. ClinCardiol. 2014;37(10): 645-649.
- Hegland, D, Kunz, G. et al A Hole in the Argument. N Engl J Med. 2005;353: 2385-90.
- Rodrigues, P, Palma, P, Sousa-pereira, L. Platypnea-Orthodeoxia Syndrome in Review: Defining a new disease?. Cardiology. 2012;123: 15-23
- Zanchetta, M, Rigatelli, G. A mystery featuring right-to-left shunting despite normal intracardiac pressure. Chest. 2005;128(2): 998-1002
- Knapper, J, Schultz, J. Cardiac Platypnea-Orthodeoxia Syndrome: An Often Unrecognised Malady. ClinCardiol. 2014;37(10): 645-649.
- Nassif, M, Lu, H. et al. Neth Heart J. Platypnoea-orthodeoxia syndrome, an underdiagnosed cause of hypoxaemia: four cases and the possible underlying mechanisms. 2015;23: 539-545.
- Christian Pristipino, Horst Sievert, Fabrizio D’Ascenzo, Jean Louis Mas, Bernhard Meier, Paolo Scacciatella, David Hildick-Smith, Fiorenzo Gaita, Danilo Toni, Paul Kyrle, John Thomson, Genevieve Derumeaux, Eustaquio Onorato, Dirk Sibbing, Peter Germonpré, Sergio Berti, Massimo Chessa, Francesco Bedogni, Dariusz Dudek, Marius Hornung, Jose Zamorano, joint task force of European Association of Percutaneous Cardiovascular Interventions (EAPCI), European Stroke Organisation (ESO), European Heart Rhythm Association (EHRA), European Association for Cardiovascular Imaging (EACVI), Association for European Paediatric and Congenital Cardiology (AEPC), ESC Working group on GUCH, ESC Working group on Thrombosis, European Haematological Society (EHA), European Underwater and Baromedical Society (EUBS), Evidence Synthesis Team, Eapci Scientific Documents and Initiatives Committee, International Experts, European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism, European Heart Journal, Volume 40, Issue 38, 7 October 2019, Pages 3182–3195, https://doi.org/10.1093/eurheartj/ehy649
- Landzberg MJ, Khairy P. Indications for the closure of patent foramen ovale. Heart. 2004;90(2):219-224. doi:10.1136/hrt.2003.019315





