What happens when a patient’s aorta falls off?
Dr M. Spurr, Dr A. Thorpe, Mr U. Benedetto and Dr M. Hamilton, Bristol Royal Infirmary.
A 41 year old man presented to a District General Hospital after collapsing three times at home. He had been experiencing headaches, double vision, and fever in the week prior. On admission the patient had raised inflammatory markers, a raised temperature and was tachycardic. The patient had a dental abscess one week before the symptoms started.
Three years previous to this admission the patient had his native bicuspid aortic valve replaced with a mechanical aortic valve and an ascending aortic replacement due to infective endocarditis (figure 1).
A transoesophageal echocardiogram (TOE) was performed which showed a large vegetation on the aortic valve replacement and suspicion of an aortic root abscess adjacent to the non-facing sinus (Figure 2). The anatomy was considered indeterminate on TOE. CT was initially turned down as it was thought it would not be diagnostic because of artefact from the aortic valve replacement. The patient was transferred to a tertiary hospital and a gated aortic angiogram CT was performed. The CT showed subtotal dehiscence of the aortic root from the ascending aorta with a large false aneurysm (see figures 3 and 4). The coronary insertion and proximal suture line of the ascending aortic replacement allowed the correct interpretation of the anatomy. While CT is inferior to TOE for showing vegetations, it is the test of choice if there is indeterminate anatomy or incompletely imaged aortic root pathology.
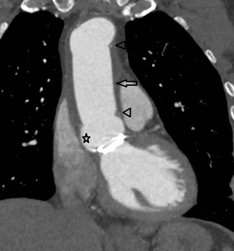
Figure 1 – Coronal oblique reformat of an aortic CT (non-gated helical). It is a baseline image from 2015 showing a post aortic valve and ascending aorta replacement
Key for figure 1
Star – sinus of Valsalva. Arrow heads – pledgets marking the proximal and distal suture lines of the ascending aortic replacement. Arrow – ascending aortic replacement.
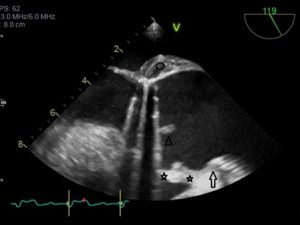
Figure 2 – Initial transoesophageal ultrasound scan demonstrating an uncertain aortic contour
Key for figure 2
Arrow – bottom end of tube graft. Stars – “2” sinuses of Valsalva. The one closest to the aortic valve proved to be a false aneurysm. Arrowhead – aortic valve vegetation. Oval – soft tissue aortic root thickening.
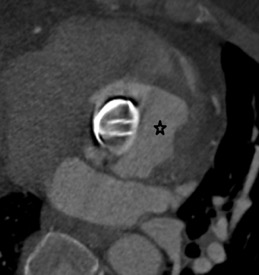
Figure 3 – Reconstructed short axis CT image of the aortic root showing the “pseudo” sinus of Valsalva (star) as a large irregular cavity around the AVR
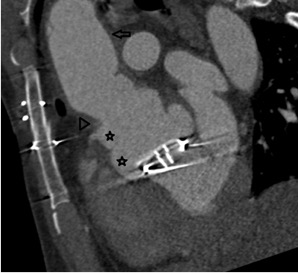
Figure 4 – Sagittal oblique ECG gated CT (systole) of the aortic root and ascending aorta
Key for figure 4
Stars – “2” sinuses of Valsalva. The one closest to the aortic valve proved to be the false aneurysm.
The patient was taken to theatre for emergency revision surgery. The aortic graft was incised and the root exposed. Direct visualisation confirmed rupture of the left sinus and an abscess associated with the right and non-facing sinus.
The previously inserted aortic graft was removed. A homograft conduit was inserted into the left ventricular outflow tract and connected distally just above the origin of coronary arteries. A tissue valve prosthesis was then implanted inside the homograft conduit. To finish a new vascular graft extending up to the proximal aortic arch was inserted.
Question 1
Which of the following statements best describes the role of CT with regards to imaging of the aortic root?
- TOE is the modality of choice when there is indeterminate aortic root anatomy.
- CT is the modality of choice to visualise an aortic valve vegetation.
- CT has no role in imaging of the aortic root.
- CT is a good alternative to visualise indeterminate aortic root anatomy if TOE is unavailable.
- CT is the test of choice for imaging indeterminate aortic root anatomy.
Answer – 5
As demonstrated by this case, although CT is inferior to TOE for showing vegetations, it is the test of choice if there is indeterminate anatomy or incompletely imaged aortic root pathology.
Question 2
Which of the following statements is correct regarding imaging of a patient with an AVR?
- An AVR is an absolute contraindication for CT imaging of the aortic root.
- CT should be avoided when a patient has an AVR as artefact will result in nondiagnostic images.
- Only a tissue valve prosthesis should be imaged with CT.
- Useful information can be obtained on CT despite artefact for an AVR.
- AVRs cause phase wrap-around artefact on CT.
Answer – 4
Useful information can still be attained despite artefact from a metallic AVR. Phase wrap-around artefact is a feature of MRI.
Question 3
What is the most common causative organism in endocarditis?
- Staphylococcus Aureus
- Streptococcus Viridians
- Streptococcus Mutans
- Escheriachia Coli
- Streptococcus Pneumoniae
Answer – 1
Question 4
What percentage of patients with prosthetic valves will develop endocarditis?
- 5%
- 1%
- 5%
- 19%
- 28%
Answer – 1
Approximately 5% of patients with prosthetic valves develop endocarditis. Involvement of the mitral valve prostheses is more frequent than that of aortic valve prostheses. (2)
References
- Murdoch DR, Corey GR, Hoen B et al.Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis–Prospective Cohort Study. Archives of Internal Medicine. 2009;169(5):463–473.
- Mylonakis E, Calderwood SB. Infective endocarditis in adults. New England Journal of Medicine. 2001;345(18):1318–1330.





